EMS whistleblowers point to major staffing concerns as thousands of Calgary zone ambulances are left vacant
New EMS data obtained from Alberta Health Services (AHS) outlines a substantial improvement in reducing “red alerts” for the Calgary Zone, in which no ambulances are readily available, but whistleblowers say the data is misleading and thousands of patients are still being left waiting for too long.
From Jan. 1 to Sept. 30, Calgary recorded 35 red alerts totalling 43.9 minutes, which is a significant reduction from the 514 red alerts totalling 712.4 minutes for the same time period in 2023.
But over the same time period, 13,325 “orange alerts” were reported in the Calgary Zone in which only one to three ambulances are left in the city, totalling 102 hours (more than four full days).
That compares with 56,862 “orange alerts” over the first nine months of 2023 totalling 481 hours (more than 20 full days).
In 2024, a total of 7,816 people who called for an ambulance during that timeframe also had their call go into “pending,” in which paramedics have not been dispatched to them until EMS has more trucks available on the road.
But the problem doesn’t stem from lack of ambulances, rather a lack of staffing.
During the first nine months of this year, 6,101 ambulances were left vacant from the Calgary Zone due to an inability to staff them.
Since January, AHS has also moved ambulances from rural areas into Calgary 978 times. That left nine of 14 rural communities without an ambulance.
“It’s obvious AHS has changed the criteria of what a red alert is by putting more calls into pending and we believe they’re doing it to avoid the publicity of relevance,” said retired advanced care paramedic Don Sharpe.
Sharpe has more than 40 years of experience working in the Calgary Zone, noting that it feels like “orange is the new red,” and says he’s never seen such a dire situation that’s being mismanaged by AHS leadership.
He also notes that the Calgary Zone EMS system has no surge capacity, which means that there are few resources available to handle the extra demand of call volumes that typically occur heading into the winter season.
“The Christmas holidays are already very tough for staffing, there’s more car crashes, more slips and falls, and more illnesses so we’re not sure if EMS can survive through it.”
“We’re running flat out every day, and I’ve seen texts from crews who have shared with me that they only have 60 to 70 per cent staffing on any given day.”
According to internal documents obtained by CTV News from the Alberta Health Services (AHS) employee portal, there are already 72 vacant paramedic shifts for Christmas Day and 95 vacant shifts for New Year’s Eve, as of Nov 13.
AHS refutes claims of misclassifying red alerts
AHS rejects claims that it’s misclassifying any red alerts as orange alerts and notes that its 7,816 pending calls “do not imply” there were more than 35 red alerts.
“Pending calls are distinct from red alerts,” read an emailed statement from AHS.
“Pending status is assigned to low-acuity calls when seven or fewer ambulances are available, prioritizing resources for high-acuity cases. Red alerts, however, occur briefly when all ambulances are in use and are prioritized for urgent calls.”
AHS also did not acknowledge that there were any concerns with staffing its ambulances despite FOIP documents obtained by CTV News that show mass ambulance vacancies in the Calgary Zone.
“Out of the 57,444 planned shifts in Calgary from January to October 2024, 89 per cent were staffed, with 51,343 shifts filled. AHS is focused on further improving demand-based scheduling while recruiting additional paramedics to address any remaining gaps,” read the statement.
“For calendar year 2023, EMS hired 470 new staff members, including 362 paramedics, and added another 296 in 2024, with 205 of them being paramedics. This has resulted in a 19.4 per cent increase in EMS staffing since December 2019.”
AHS maintains it is actively recruiting new paramedics while also focussing on “retaining its dedicated staff” through a multifaceted marketing campaign targeting local, national and international audiences which was launched from October 2023 to March 2024.
“The campaign has already garnered 905 responses from interested candidates and 2,152 unique applications,” AHS said.
‘Where are these new hires?’
The large void in the roster is prompting some paramedics to speak out against their employer.
One paramedic spoke to CTV News anonymously due to fear of reprisal at work said they’ve been pushed to the limit.
“They (AHS) just kind of flipped the policy on its head, and now all of a sudden, they’re stacking calls or putting calls into pending before they actually call a red alert,” the paramedic said.
“You’re just tired all shift long. You go to the hospital to clear up and there’s already 10 calls waiting because crews are either stuck in the hospital or they don’t have the people to staff the ambulances.”
The paramedic was shocked by the AHS statement that staff has increased 19.4 per cent since December 2019.
“Where are these new hires? What they’re hiring is essentially a leaky bucket because they’re losing more people than they’re actually bringing in. I don’t run into a lot of new recruits. I can have unlimited overtime right now if I want,” they said.
“It’s very disheartening seeing all the gaslighting from upper management or senior leadership and the way that they think that we’re going to celebrate these achievements that they’re purporting, that we’re experiencing when the reality on the street is not what they claim.”
AHS notes that it is aware of the capacity pressures at hospitals and has since implemented what it calls “dedicated inter-facility transfer (IFT) resources” through contracted partners to hand low-acuity transfers.
“This is allowing patients to return to their communities sooner and freeing up AHS EMS ambulances for emergency calls. In Edmonton and Calgary, these additional resources are now handling 400 transfers per week, significantly alleviating pressure on EMS,” AHS said in a statement.
“AHS also introduced the EMS Return to Service initiative, designed to quickly return frontline EMS crews to the community while ensuring safe and efficient patient transfers. This initiative includes improved coordination between frontline staff, EMS supervisors, ED triage, site leadership, dispatch, and hospital teams to enhance access and patient flow.”
‘My father deserved an ambulance’
For Erin Graham, the delays tell a more personal story.
On New Year’s Eve of 2021 she called an ambulance for her ailing father, but it never arrived in time to help him.
“I really miss my dad. He was a farmer, a really simple guy who loved the simple things in life, but when he needed an ambulance, it wasn’t there,” she said.
“My father deserved an ambulance.”
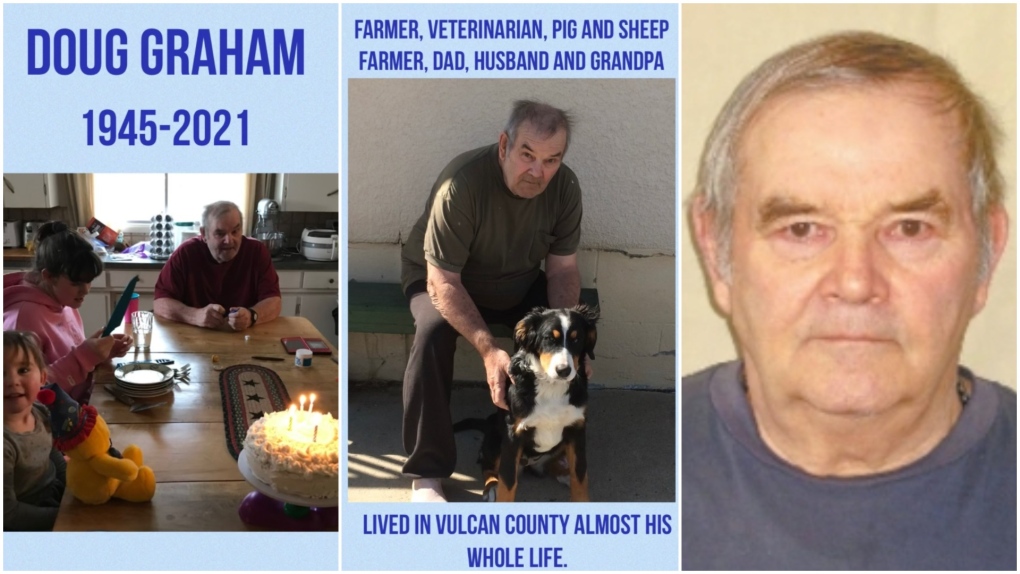 Photos of Douglas Graham, of Vulcan, Alta., who died on New Year’s Eve 2021. (Courtesy: Erin Graham)
Photos of Douglas Graham, of Vulcan, Alta., who died on New Year’s Eve 2021. (Courtesy: Erin Graham)
Erin’s father, Douglas Graham of Vulcan, Alta. died at the age of 76 following a battle with COVID-19.
“He obviously had a stroke because we couldn’t lift his feet into the car to take him to the hospital and that’s when he fell down outside. It was minus 28 out there and we were told there wasn’t an ambulance in the Vulcan County so we had to wait 45 minutes,” Graham said.
“About 20 minutes into waiting, my dad stopped breathing and he didn’t have a heartbeat anymore. It was a disaster and I just started doing CPR. Finally, I hear the ambulance come but my dad had been dead for least 20 minutes at the point. Had they come from Vulcan, they definitely could have saved him.”
Graham will never know if medical care arrived more quickly whether it would have ultimately saved his life.
But she says she was told that that no ambulance was available in her community or region as they were all dispatched elsewhere. The closest ambulance was a 45-minute drive away at the time of her call for help.
View original article here Source









