Names of Ontario health-care clinics found to have extra-billed being kept secret
The names of physicians and facilities found to have engaged in extra-billing for health services are being kept secret, with advocates arguing this lack of transparency could impact public trust in the health-care system.
Data obtained by CTV News Toronto through a freedom of information request found that 183 complaints were made about extra-billing in Ontario between January 2021 and Dec. 30, 2022.
Of those complaints, 49 were found to have contravened the Commitment to the Future of Medicare Act (CFMA).
These contraventions included extra-billing for health services that should have been covered under the Ontario Health Insurance Plan (OHIP) to the tune of just over $68,000.
But the physicians or facilities that charged patients for these services are unknown. The government redacted the service providers’ names, as well as the facility name.
They argued the disclosure of the records could prejudice the competitive position of a person or organization, and therefore, are exempt from freedom of information laws.
CTV News Toronto is currently appealing to obtain the information in part.
When asked why the information could not be disclosed, a spokesperson for the minister of health said that violations related to extra-billing may be unintentional or the result of a misinterpretation by a provider or staff.
“When a CFMA investigation finds a provider to be in violation of the CFMA, the ministry works with the provider to give them the opportunity to be in compliance with the Act, so they can continue their operations,” they said in a statement.
The ministry also argued the information cannot be disclosed by law.
“I don’t think the public interest is served by redacting that information,” Andrew Longhurst, health policy researcher at Simon Fraser University and research associate at the Canadian Centre for Policy Alternatives, told CTV News Toronto. “I think part of an enforcement regime means having to name and identify those that are engaging in unlawful behavior.”
Longhurst has reviewed similar data spanning two decades, and in each case the same identifying information has been left out. He says the data is “very much an under-representation” of the number of unlawful extra-billing occurring in Ontario, given the system is entirely complaint-driven.
“It’s not a proactive regime,” he said. “I think a lot of patients often are in a state of kind of surprise or shocked (and) don’t really realize that this is actually an unlawful illegal practice.”
Between January 2003 and April 2023, there were 2,884 complaints made about extra-billing. Of those, just over 31 per cent, about 916 complaints, were found to have violated the CFMA.
The data from 2021 onward shows patients paid – and were reimbursed for – eye exams, dental extractions, the removal of stitches, the injection of drugs, and in one case a vague “health card initiated charge.”
“I think it needs to be taken seriously by the government, especially as you introduce greater for-profit involvement,” Longhurst added.
In May, the Doug Ford government passed legislation allowing for-profit and not-for-profit clinics to conduct more OHIP-covered procedures, including cataract surgeries, MRI and CT scans, minimally invasive gynecological surgeries, and knee and hip replacements.
They insisted that patients would not need to pay for these services out of pocket.
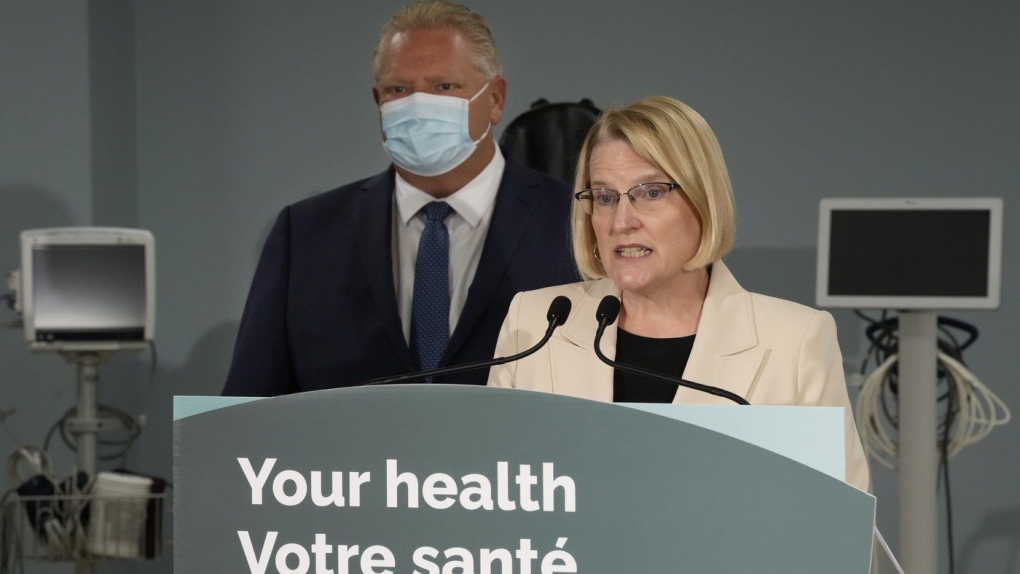 Ontario Health Minister Sylvia Jones makes an announcement on healthcare with Premier Doug Ford in the province in Toronto, Monday, Jan. 16, 2023. THE CANADIAN PRESS/Frank Gunn
Ontario Health Minister Sylvia Jones makes an announcement on healthcare with Premier Doug Ford in the province in Toronto, Monday, Jan. 16, 2023. THE CANADIAN PRESS/Frank Gunn
As of January 2024, the Ministry of Health said more than 900 community surgical and diagnostic centres were operating in Ontario. This number is expected to increase in spring to allow for additional MRI and CT scans, GI endoscopies and orthopedic surgeries to be completed.
The ministry did not say how many additional centres would be given the green light.
In January, the province also named Accreditation Canada the inspecting body responsible for ensuring quality and safety standards. A spokesperson said this month that the organization is “in the early stages of designing an assessment program with the Ontario Ministry of Health.”
More information on the licensing process will be released closer to the program launch date on April 1, the spokesperson said.
As it stands, data available on the government’s website says that 112 of community surgical and diagnostic centres have either not been assessed under current ownership or require a follow-up assessment.
All other clinics have been found to have “met standards.”
Accreditation Canada confirmed that its program focuses on “patient safety and quality care delivery” and not issues related to billing. Those concerns are under the purview of the ministry of health.
What is extra-billing?
The government’s decision to allow more independent clinics to conduct surgeries was met with nearly immediate criticism from health-care unions, advocates, and opposition leaders who claimed it would not only squeeze staff from hospitals, but it would also result in manipulative upselling of medically unnecessary services.
A patient is extra-billed when they are asked to pay for a service covered by OHIP, charged fees for items like overhead costs, or are pressured into purchasing upgraded devices they don’t need.
“The occurrence of billing issues was something I didn’t anticipate that we’d be dealing with right out of the gate when we opened the office, it was eight years ago,” Ontario’s patient Ombudsman Craig Thompson told CTV News Toronto in an interview.
Some of the more common complaints, Thompson said, surround upgraded hospital accommodations and ambulance transfers.
He acknowledged that with the addition of more community surgical and diagnostic centres, he has heard concerns about upselling, noting that it is possible for some patients to sign up for something they don’t quite understand.
The Ministry of Health noted that most of the CFMA violations have not occurred at independent clinics, saying that “over the past three fiscal years of data, community and surgical diagnostic centres did not have any violations of the CFMA where as hospitals, physicians and other providers had multiple violations.”
However, prior to 2023, there were significantly less independent facilities registered with the government.
 Healthcare workers’ personal protective equipment hangs at a clinic in Sarnia, Ont., on Wednesday, January 26, 2022.THE CANADIAN PRESS/Chris Young
Healthcare workers’ personal protective equipment hangs at a clinic in Sarnia, Ont., on Wednesday, January 26, 2022.THE CANADIAN PRESS/Chris Young
Under the new Integrated Community Health Services Centres Act, it is illegal for a service provider to offer preferential treatment in exchange for payment or to ask a patient to pay for a service covered under OHIP.
However, if the Ontario patient ombudsman receives a complaint and finds a violation, all they can do is offer mediation and make recommendations.
“It’s a more informal process at the front end when we get a complaint, because the best resolutions always are the ones that are timely, and happen as quickly as possible,” Thompson said.
The process involves working with both parties to come to a solution, whether it’s an apology, a policy change or training.
“But at the end of the day, there’s nothing in law that allows us to compel those organizations to act on anything that we recommend,” he said. “But we have a very good track record with working with our organizations to understand that the fairest processes are the best processes.”
Should names of violators be kept secret?
Thompson says that in order to get the best results for the complainant, he doesn’t believe it would be productive to “name and shame.”
“In the vast majority of situations, organizations and the staff, and leadership within those organizations want to do a good job of delivering health care,” he said. “So once it’s brought to their attention that there’s been a problem … then they’re more than happy to make a change in a process, make a change in a policy, do some training for staff.”
“And at that point, we have essentially achieved what typically that complainant wants is that that situation not to occur for somebody else in the future.”
At the same time, he said it would be “totally appropriate” to name a bad actor who is consistently breaking the rules.
Ontario NDP Health Critic France Gélinas, however, disagrees. While she noted that mistakes can happen, and that “at the core of every physician, there’s a human being who is not perfect,” she thinks the benefits of naming service providers found to have violated the CFMA trumps the risks of not doing so.
“When you know that there is no oversight, when you know that there is no transparency, there’s a lot less pressure on people to do the right thing,” Gélinas said.
“This trust is something we need in our health-care system. When you start to lose trust in your health-care providers, it becomes really hard to provide quality care.”
Not only does Gélinas believe that service providers should be named, but she would like to see a follow-up investigation take place to see if any other patients were similarly billed.
“If you’re coming to Ontario to make money off the back of sick people through loopholes, through having them sign documents that they can’t even read because they need cataract surgery, then we will shut you down.”
View original article here Source









